The United States is facing an increase in human infections by drug-resistant bacteria. One such bacteria, called New Delhi metallo-beta-lactamase-producing carbapenem-resistant Enterobacterales, is considered especially dangerous due to the fact that the bacteria are “resistant to some of the strongest antibiotics available.”
Enterobacterales are a group of bacteria that exist normally within the gut of humans and animals; however, they also have the potential to cause infection. Common species of enterobacterales include Escherichia coli, Klebsiella pneumoniae, Enterobacter cloacae and Citrobacter freundii. Carbapenem-resistant Enterobacterales are bacteria that have resistance to one or more antibiotics, like carbapenems, which are often considered the “last-line” treatment for serious drug-resistant bacterial infections.
Enterobacterales can gain carbapenem resistance through a variety of methods. One such method is via the production of carbapenemase, which is able to break down carbapenems. In the case of NDM-CRE bacteria, they produce an enzyme called New Delhi metallo-beta-lactamase, which causes resistance to a wide range of antibiotics, including carbapenems. NDM-CRE can cause infections, including pneumonia, urinary tract infections and bloodstream infections.
The Centers for Disease Control and Prevention published a report on Sept. 23, noting an over 460% increase in NDM-CRE infections between 2019 and 2023 that resulted in many difficult-to-treat infections. It is also notable that this report is not the first that the CDC has produced on CRE and NDM-CRE infections in the country. In 2022, the CDC reported roughly 12,700 infections and 1,100 deaths due to CRE. Another report earlier this year highlighted an increase in NDM-CRE infections from 58 in 2019 to 388 in 2024.
What is more concerning about the new CDC report is that the researchers did not obtain data from many highly populated states, including California, Florida, New York and Texas, in their calculations. Due to this, Assistant Professor of Medicine Jason Burnham of Washington University in St. Louis believes that the number of infections is “definitely underestimated.”
NDM-CRE bacteria were previously considered uncommon in the United States, and there are not many treatment options available. Researchers have noted that only two antibiotics are known to work against NDM-CRE infections. However, these antibiotics are expensive and must be administered intravenously, meaning they cannot be taken orally and typically must be administered in a healthcare setting. This leads to more complications when thinking about the feasibility of treatment options.
CDC epidemiologist Danielle Rankin highlights that “there is risk that this could spread into communities, meaning that common infections like urinary tract infections that are usually treated with the oral antibiotics may increasingly need to be treated with the IV antibiotics and require hospitalization.”
Another major barrier to care for patients and control the spread of infection is due to the fact that the tools available to detect NDM-CRE infections are not often found in healthcare settings since this was not previously a major concern. Furthermore, individuals with NDM-CRE are asymptomatic until an infection develops, and from this, the symptoms that the individual will experience are varied based on the infection. By ensuring “healthcare providers have access to testing,” providers will have an increased ability to choose appropriate treatment, Rankin said.
According to the CDC, researchers are still working on understanding all of the reasons for this increase in cases of NDM-CRE infections. Potential causes of NDM-CRE infections include the overuse of antibiotics. Susan S. Huang, professor of infectious diseases at the University of California Irvine School of Medicine, explained that unnecessary use of antibiotics leads to the death of healthy gut bacteria, allowing room for bacteria like NDM-CRE to multiply. Huang believes that an increase in antibiotic use during the COVID-19 pandemic may have played a role in this increase of NDM-CRE. The CDC reported that 80% of patients hospitalized with COVID-19 from March to October 2020 received an antibiotic. “Never before had so many antibiotics been prescribed for a viral disease,” Huang wrote.
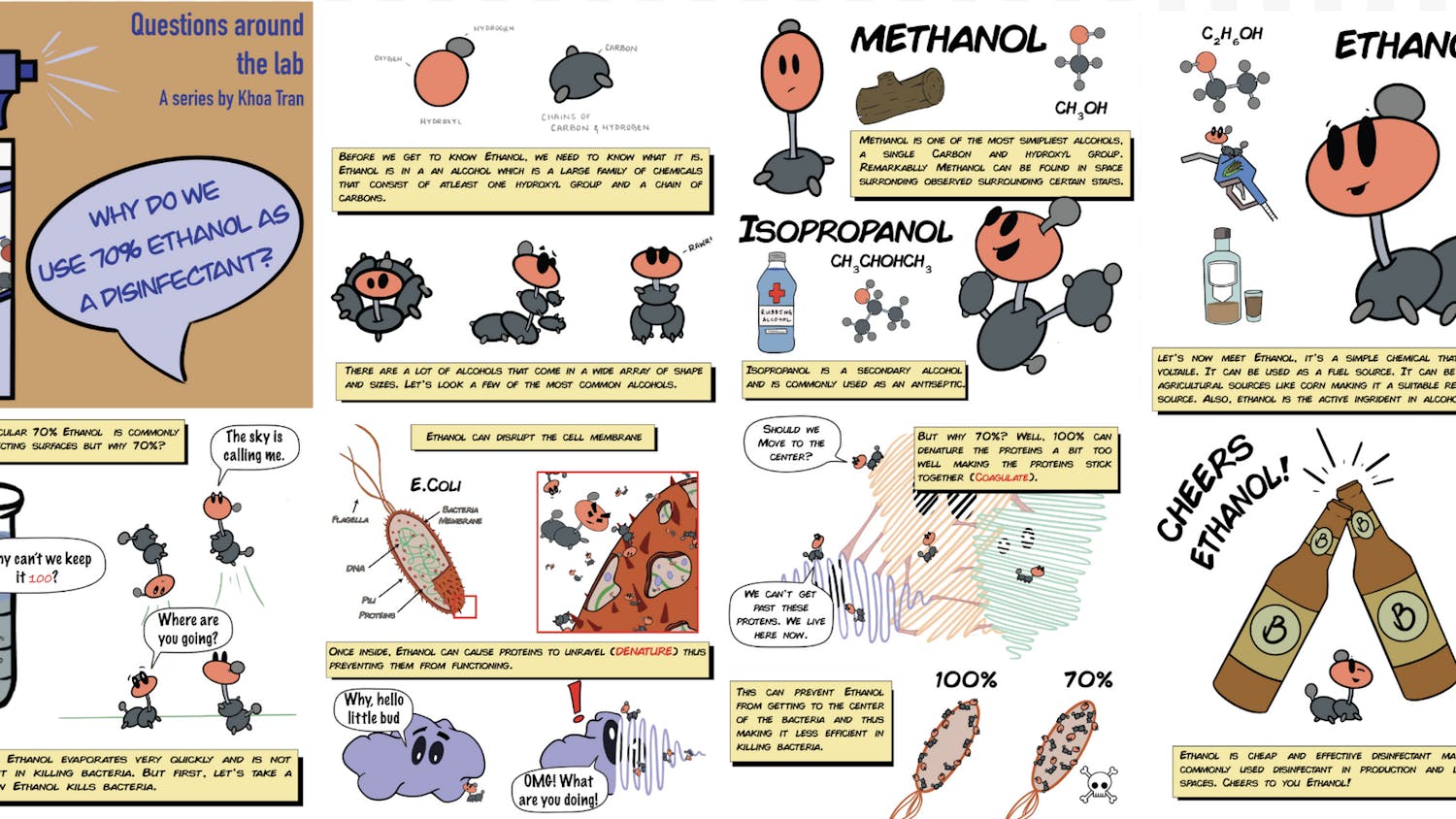
NDM-CRE bacteria can be spread through contaminated surfaces, and, hence, spread can be caused by inadequate hand hygiene and disinfection of surfaces. Healthcare professionals, patients and visitors in hospital settings are encouraged by experts to frequently wash hands and avoid contacting any potentially contaminated surfaces. Those most at risk include people who have taken many antibiotic courses, people in hospitals who have had repeated or long stays and those who have been in contact with someone who had an NDM-CRE infection. As research continues to be uncovered about the NDM-CRE bacteria, it is important to stay informed and updated.